The Pressure is On
Healthcare systems in the US are facing substantial financial challenges. Since the Covid-19 pandemic, factors such as labor shortages, supply chain interruptions, and macro-economic pressures have all compounded the already mounting cost pressures. Over the same period, government reimbursement increases have not been adequate: while the economy-wide inflation in the US grew by 12.4% between 2021 and 2023, Medicare reimbursements for hospital inpatient care only grew by 5.2%.1
In parallel, there have been several developments upending the very fabric of the US healthcare ecosystem. In the past, hospitals could depend on passing increasing costs of care to payers; however, with the transition from a volume-based to a value-based business model, this will no longer be the case. Rising costs pose a considerable challenge for hospitals that aim to maintain equal access to care while maintaining investments in cutting-edge treatments and technology. As a result, healthcare organizations are increasingly seeking ways to intelligently optimize their cost base without compromising quality or access. Given large healthcare organizations typically operate on margins of 1-3%, adopting a strong cost-conscious approach is not only prudent but survival critical.
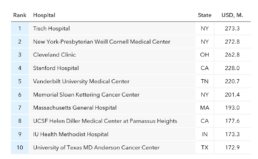
The focus of this whitepaper is tech-related spending and budget transparency. Within healthcare organizations, the largest category constituting the internal cost structure2 are labor (60%), supplies (13%), and drugs (8%). Technology-related spending – a category that is not a direct patient care service, but that is nonetheless critical for delivering care – stems from costs associated with implementing, maintaining and upgrading information management systems and technology operating budgets. For large healthcare systems, technology-related spending represents investments of up to 4% of revenue2 (Exhibit 1) of which the largest categories are typically infrastructure maintenance, electronic health records (EHR) support, and cybersecurity & resiliency (which has seen an increase as of late, due to frequent ransomware attacks targeting hospitals).
Exhibit 1. Healthcare technology operating budget
& directional breakdown by category
2017–2022
Given the substantial spending on technology (Exhibit 2), IT teams are increasingly being called on to explain and justify their budgets. However, IT teams usually face two challenges when trying to demonstrate the efficacy of their spending due to:
- Absence of technology mappings: Historically, the approach to cost transparency and allocation within healthcare organizations has differed from that in other industries. Following a “non-business” philosophy, IT has often been treated as overhead, and rarely were application or infrastructure costs tied back to any business verticals or services. As such, these mappings were never required previously.
- Nascent standardization and reporting: This inability to treat costs as service inputs and allocate them accordingly makes it difficult to provide granular views of the areas where the budget used. As a result, IT teams struggle to communicate the value they provide to the business lines when justifying their total expenses. The absence of standardized services renders IT incapable of providing the business and the clinicians with levers to enable them to help control cost and consumption.
To better manage their products and services, healthcare providers must establish transparency and identify the underlying cost drivers of the services they deliver. Understanding the unit costs of delivering IT services is crucial to identifying performance and cost variability, isolating cost drivers, and achieving commercial excellence.
This whitepaper outlines how healthcare organizations can create clarity and transparency when it comes to their service offerings. It will further demonstrate how organizations can effectively allocate and manage their IT expenditures. Specifically, section 2 will first examine the case for cost transparency and shed light on the biggest challenges encountered by hospitals; section 3 paints the vision for a target state as well as interim transition stages towards IT cost transparency, including the need for business-aligned KPIs; section 4 introduces five steps to embark on the journey of services definition and cost allocation. Finally, we conclude with a summary of how third parties can help with planning and executing the total cost of ownership (TCO) journey.
Exhibit 2. U.S. hospitals with highest 2023 operating budgets4
A Strong Case For Transparency
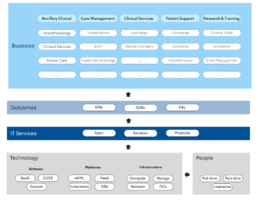
Compared to healthcare organizations, companies in other sectors such as financial services tend to have a clearer understanding of their underlying cost structure. Traditionally, companies in these sectors are acutely aware of the costs involved in providing their products and services. This is because they must determine what customers will pay for this product or service, and what the resulting margins will be. Moreover, other sectors often have a more detailed view of the business activities that support their operations, such as the cost of technology, finance, and supply chain management. Partially driven by the abstraction of accountability in the US healthcare hybrid system (i.e., multiple-payer, single-payer, and socialized medicine elements), this level of awareness has not traditionally existed in healthcare. With the transition of the healthcare industry from a volume-based to a value-based model, healthcare administrators are beginning to pay closer attention to unit costs, recognizing that both patients and insurers will increasingly care and inquire about these costs. A comprehensive, end-to-end cost view as shown in Exhibit 3 is needed.
As healthcare leadership aims to streamline and simplify the healthcare operating model, they are looking to make decisions based on cost; however, there often is not enough cost transparency, which limits the ability of organizations to (1) know what IT services and assets cost the hospital today, (2) streamline solutions to eliminate redundancy, and (3) understand the competitiveness of the services they offer. For research hospitals, another challenge arises in the context of external grants. For these, hospitals usually charge a processing fee on grants for the institutions; this fee can then cover access to hospital resources such as office space and IT support. Given the already enormous demand and hefty price tag for AI research resources such as storage and compute, hospitals must be able to tie these costs back to the individual research projects to ensure fair and equitable accounting.
Exhibit 3. End-to-end View Connecting Business
Services And Technology Cost Pools
Establishing transparency and a robust methodology to allocate IT costs back to the services they support, therefore, allows for a multitude of activities, all of which are crucial in an environment where IT plays an ever-larger role and competition becomes fiercer. Once transparency and control are established, IT organizations will be better positioned to support their organizations on multiple fronts (Exhibit 4):
- Provide customers with expertise on technology investments
- Proactively & continuously rationalize technology portfolios
- Maximize the organizations return on investment for IT
- Understand the customer demand and challenges
Exhibit 4. Healthcare Provider Business Services (illustrative)
Setting the Vision
Eventually, healthcare organizations should be able to track their costs by category (e.g., resources, IT) and to be able to roll them up to each of their individual business services. To achieve this goal, the IT organization needs to capture detailed IT metrics such as app cost per user, storage cost per terabyte, server cost per CPU and/or RAM, and labor cost per application. These costs should then be bundled as IT services, quantitatively tracked, and allocated to various, clearly defined services at the business level.
This mapping allows for granular reporting and enables infrastructure managers to clearly illustrate the cost of computing to finance and business leaders. As a result, all parties will be better able to engage in meaningful discussions about various technology solutions and have a better understanding of the trade-offs involved, including the awareness of IT’s capacity limitations. Once transparency has been established, a conceptual shift in the interaction model between the business verticals and IT can occur. The conversations can shift from “IT is too expensive” to “how technology consumption is driving these costs.” Enabling IT to share application data with internal customers, including doctors, nurses, and executives outside the IT organization will facilitate business-driven decision-making in partnership with these internal customers regarding which applications should be rationalized and retired. Exhibit 5 provides and overview of the maturity journey that organizations usually go through when establishing cost transparency.
Exhibit 5. Innovation Adoption for Healthcare Organizations
Getting Started
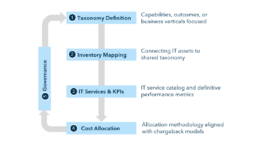
Depending on an organization’s exact starting point, establishing IT cost transparency to ensure alignment of spending with overall business priorities can be a substantial undertaking. In this section, we lay out our 5-step approach for realizing this goals while delivering interim milestones, such as asset mappings and services taxonomies.
One of the first and most essential tasks towards ensuring alignment of the business and IT is to establish a shared taxonomy and adopt consistent definitions. This need for defining clear service hierarchies to serve as a common denominator pertains to business verticals and corresponding services (e.g., clinical, patient care) and IT offerings (e.g., platforms, applications, EUC support) alike. Agreeing on a shared taxonomy ultimately allows for complex relationships to become tangible and enables healthcare organizations to make coordinated, data-driven decisions aimed at maximizing business value.
In the five steps that follow (Exhibit 7), we have included key considerations and lessons learned from our experiences in helping healthcare organizations succeed in implementing cost transparency and optimizing their spending. These steps cover setting up a shared taxonomy, mapping of in-scope assets, defining the scope of IT services, and setting up a cost allocation mechanism.
Step 1: Defining Taxonomies
When defining the provider business taxonomy, focus on the outcomes or services that the business verticals should deliver, without specifying tools, processes, or methods. These definitions should be stable and adaptable, maintaining consistency despite changes in personnel, processes, or technology. Additionally, alignment with internal practices and industry standards is needed for coherence.
- Inventory: List current services (e.g., clinical) and sub-services
(e.g., audiology, bariatric surgery) following standardized verticals - Hierarchy: Map each service to its corresponding sub-services
- Meta Data: Capture service attributes (e.g., owner, description, activities, customers)
Step 2: Inventory Mapping
Once a shared taxonomy is established, map all assets (applications, databases), to the corresponding services. This mapping will cover both one-to-one (e.g., sub-service specific application) and one-to-many relationships (e.g., shared HER system), providing a foundation for linking IT assets with business activities.
- Functionality: Capture primary function of each in-scope asset (e.g., apps, platforms)
- Ownership: Validate asset-specific ownership and identify other relevant stakeholders
- Mapping: Capture relationships of in-scope assets and business services / sub-services
Step 3: Establishing IT Services & KPIs
In the third step, the IT organization should define how it delivers value, outlining the IT-specific services that will be provided to support business operations. Each IT service should be measurable, with specific KPIs and/or OKRs, to allow for accurate tracking of performance and measurement of improvements over time.
- Service Catalog: List all IT services provided to customers
- KPIs: Define measures for each IT service (e.g., performance)
- Ownership: Establish ownership for each IT service to ensure accountability
Step 4: Cost Allocation & Chargeback Models
The fourth step focuses on identifying cost elements, developing an allocation methodology, and establishing a mechanism that aligns costs with consumption and business value for the different business functions. Various models exist, and the selection (e.g., overhead, show back, pass-through, chargeback) should occur in accordance with the organization’s aspiration for cost recovery, accountability, and control.
- Levers: Identify cost elements for each sub-service (e.g., apps)
- Allocation: Develop methodology for costs (e.g., by usage)
- Cost Pools: Identify cost pools based on type (e.g., infra, software)
- Categorize: Determine cost pools and attribution by period
Step 5: Continuous Governance
In the final step, the organization needs to setup the required governance and operational processes to ensure that cost allocation & reporting mechanisms are kept up to date and can evolve over time. In a fashion not unlike traditional ITSM processes, there should be provisions for major events, such as the introduction of new services, service changes, and service retirement. Additionally, there should be a governance cadence to oversee the program and review success metrics periodically and adjust as required.
Exhibit 7. Five Step Process for Getting Started
In Closing...
Increasing costs and stagnating prices have resulted in an environment of financial uncertainty. Most larger health systems are operating with little to no profit margins. As of today, hospitals are far from where they need to be to meet the demand for care while investing in new technologies. In this context, to achieve commercial and operational excellence for technology, organizations must enable processes that allow them to track and manage technology costs proactively and to demonstrate business value realization.
At Kepler Cannon, we are committed to being the catalyst for our customers’ journeys towards cost transparency. We work closely with our clients to understand their goals and then develop the most effective plans to enable CIOs and CFOs to assess the added value of their IT services and investments based on data. Leveraging our frameworks and repositories, we accelerate preparatory work and design and implement allocation and attribution methodologies. Our comprehensive best practices ensure the creation, maintainability, and upgradability of a holistic IT cost view, encompassing all business and technology services.
Whether you are just starting your journey toward cost transparency or looking to optimize an existing cost allocation and attribution process, contact us today and let us know how we can best support you.