Wave of Platformization
Platformization has emerged as a pivotal trend, particularly in highly fragmented sectors such as healthcare, which features over 4,000 software vendors.(1) Healthcare organizations are often so fragmented, it is not unusual for companies to need 300+ isolated point solutions for their day-to-day processes.(2) This proliferation of apps significantly increases the need for integrations, all while IT budgets become more constrained from multiple subscriptions to different point solutions.
Across industries, large technology firms such as Salesforce, ServiceNow, and Workday are responding to this need for consolidation and leading the wave of platformization through strategic acquisitions and rapid development. For instance, Salesforce has developed features for customer engagement and servicing, employee collaboration, and analytics into a single solution. This shift has prompted companies across sectors such as Spotify, Humana, and Royal Bank of Canada to migrate to Salesforce, resulting in a 40% increase in sales productivity.(3) Similarly, ServiceNow offers a comprehensive IT Asset Management platform, streamlining everything from asset onboarding to cost management. Additionally, Workday consolidates human resource functions, providing integrated services in human capital and talent management, enhancing efficiency and reducing vendor complexity.
With these consolidated platforms, organizations are able to achieve greater synergies and interoperability for an all-in-all easier to use, more comprehensive system. This expansion of offerings has occurred over time to create a cloud-first, modern, customizable, and integrated system for end-to-end processes.
Exhibit 1. Evolution of Platforms
The Disjointed Healthcare System
While significant progress has been made, healthcare remains hindered by outdated and fragmented systems.
1. INSURERS
–For example, regional payers processing over 5 million medical claims annually use about 5+ vendors for claims adjudication alone. This is often supported by 50 additional vendors for other services such as file transfers, payment processing, and more.(4)
–Another payer manages over 2 million medical claims but restricts their all-in-one vendor to only two functions (e.g., claims processing and utilization management). However, they rely on custom-built solutions for other needs.(4)
Maintaining a fragmented system dramatically increases IT costs for claims processing, with the cost being 250% higher than more modern, integrated solutions. Additionally, to manage these systems, organizations often require 80% more personnel than industry norms.(4)
2. PROVIDERS
–On the provider side, many healthcare systems operate with 10-20 essential functions, such as administration and clinical operations, but are burdened from using hundreds of different systems to support all processes.
Driven by the burden of managing hundreds of vendors and the corresponding costs of doing so, healthcare organizations should be compelled to modernize and streamline their technology ecosystems.
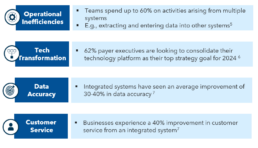
Exhibit 2. Case for Platformization
Ripple Effects of Silos
The impact of siloed systems used in the healthcare industry extends widely, significantly affecting operational efficiency. Here’s how:
1. Data Fragmentation: Disconnected systems across different departments create data silos, hindering access and leading to outdated, duplicated data. Managing outdated and duplicated data costs 30% of total labor expenses, risks 4% of revenue in compliance, and further reduces revenue through inefficiencies.(8)
2. Tech Incompatibility: Using multiple vendors often requires a foundational connectivity layer. Established vendors often provide ready-made connections, whereas lesser-known vendors might require expensive custom builds to ensure compatibility. This can delay timelines and pose risks, with one in six companies reporting projects running 70% over schedule and 200% over budget.(9) This is particularly troubling for healthcare where compliance and strict deadlines outlined by regulators (e.g., CMS and state Medicaid) must be followed, or payers risk losing member contracts.
3. Manual Intervention: With so many systems, users are required to manually transfer and re-enter data across different platforms. This is not only time-consuming and error-prone, but also delays critical business decisions. Evidence suggests that organizations face annual losses of over $3 million if over 50% of a full-time employee’s workload is spent manually coordinating between systems.(10)
4. Resource Drain and Productivity Losses: Using many point solutions requires a larger technical staff dedicated to ongoing system integration and forces business professionals to focus on workarounds rather than their primary duties. Consequently, each new system update or technology introduction increases workload, stress, operational costs, and diminishes productivity.
5. Compromised Security: Each integration or communication layer adds a potential entry point for attacks, increasing the risk of compromised system security.
6. Limited Scalability: Fragmented infrastructure, data silos, manual processes, and a lack of standardization hinder the ability to scale technology. This is particularly problematic in healthcare, where growing patient and claims volumes demand robust, scalable systems.
7. Regulatory Non-Compliance: Data fragmentation and inconsistencies create incomplete audit trails, risking non-compliance with regulatory standards. Inconsistent data security protocols across various vendors can expose systems to cyberattacks, jeopardizing patient data and potentially resulting in costly HIPAA fines ranging from $100 to $50 thousand per violation(11).
8. Rise of Additional Vendors: Healthcare organizations frequently engage professional services to develop workflows and manage data fragmentation, leading to increased costs and increasing the number of vendors in the ecosystem.
Future of Connected Healthcare
Fragmentation persists both within and across payer and provider systems, affecting operations from core to surrounding segments. For payers, navigating the complex interdependencies of the value chain and the numerous entities involved, as detailed in Exhibit 3, is a nightmare in the absence of Platformization. For example, in insurance, the claims teams often manually inputs prior authorization data, constructs custom workflows to share finalized claims with state regulators and more.
These stopgap measures contribute to delays and a cascade of problems such as coding errors, repeated manual adjustments, and processing inaccuracies, leading to penalties upwards of $3 million9, elongated processing times, and lower auto-adjudication rates. Even for providers, a lack of a centralized source for patient data combined with no downstream connectivity with payer systems can lead to oversights in patient care. Vendors are actively consolidating systems and processes both across and within payer and provider domains to mitigate these issues. However, adoption rates for such solutions are still sub-optimal.
Exhibit 3. Payer Value Chain(12)
Exhibit 4. Modular Platformization of Healthcare
Consolidation efforts on integrating previously siloed functions, as demonstrated in exhibit 3, into fully configurable modules detailed in exhibit 4 are visible across vendors of various sizes and archetypes. For example, prominent ‘Pega-shops’ are leveraging their technological expertise and scalability to undertake comprehensive in-house custom builds. Players are also investing in acquisitions to expand scope of offering. For example, Oracle’s Health Insurance Cloud’s recent acquisition of Cerner, a leading EHR, showcases its expansion into both payer and provider domains.
Similarly, major professional services providers are acquiring companies to offer integrated products with adaptable modules, as illustrated by Cognizant’s acquisition of TriZetto. Even smaller professional services firms that started off as consultants for patching operational gaps, are now broadening their offerings to include consolidated healthcare products. Moreover, providers like Epic Systems, traditionally known for their EHR systems, are venturing into payer solutions, adding functionalities such as portals, enrollment, authorization, and utilization management tools.
Embracing Integrated Solutions
Integrated solutions can help organizations experience cost savings, data integrity, and a unified user experience.
1. Cost Savings: From a reduced number of licenses, streamlined maintenance and support, minimized training across different platforms, and simplified vendor management, organizations can experience significant cost savings.
2. Increased Data Integrity: As a result of one vendor, a “source of truth” with standardized data formats helps to decrease data silos and the need for manual entry into multiple systems.
3. Unified User Experience: A single interface across various process steps reduces the need to switch between systems and search for missing or outdated information, leading to a more unified user experience.
4. Single Point of Accountability: With one vendor, challenging scenarios such as system downtimes can be resolved quicker with the need to only work with that vendor. Additionally, using a broader range of services from a single vendor can strengthen relationships, which is vital for timely issue resolution.
Beyond the immediate benefits outlined above, there are substantial long-term benefits to be gained from establishing a strong partnership.
In healthcare, where platform procurement is a long-term commitment, it is essential for organizations to look beyond immediate financial benefits and choose a partner that not only supports but also actively guides their growth journey.
Below is how organizations should think of long-term partnership gains:
1. Premium Customer Support: Utilizing a broader array of services from a single vendor often leads to higher quality support. When one vendor is familiar with most of your operations, it can more easily identify issues. This also gives the organization greater influence over improvements and enhancements.
2. AI Leverage: Vendors continually invest to enhance their offerings. By adopting consolidated platforms, organizations can capitalize on vendors’ AI investments, which often include pre-built AI models and robotic processing automation. This comprehensive approach allows for more extensive improvements across the entire value chain, rather than just parts of it.
3. Pre-Built Market Integrations: Vendors that expand through consolidation often provide pre-built market integrations for areas of the value chain they have not ventured into yet that organizations can benefit from.
Still Not Foolproof
The choice to transition to a consolidated platform is not straightforward. Despite the potential benefits, adoption by both payers and providers remains measured.
1. Data Migration Issues: Point solutions often result in fragmented, non-standardized data. As a result, migration can be a daunting task. Furthermore, healthcare data is subject to strict privacy, security, and confidentiality regulations under HIPAA that organizations must adhere to during migration.
2. Vendor Lock-In: With a single vendor, organizations are heavily dependent on it for support, updates, and maintenance. If the vendor experiences issues (e.g., software, security), it can be extremely disruptive to the organization. However, these issues are rather rare and be combatted by baking in strong contractual terms.
3. Parallel System Maintenance: Migrating to a modern system often necessitates running old and new systems concurrently, leading to temporary high costs and increased employee workload from managing dual systems alongside their regular duties. To mitigate this, organizations need to plan and allocate resources accordingly.
4. Stringent Timeline: Payers must pay attention to the timing of their system migration. Insurers need to consider Medicare/Medicaid bid years, as regulators prefer to award business to organizations that are not in the middle of changing their technology stack.
5. Resistance to Change: Even with fragmented systems, users often grow comfortable with the wraparounds and manual inputs. Users often develop a resistant mindset, even if the change is to a more friendly system. Successful platform integration requires comprehensive change management, including extensive training and post-implementation support.
Even if organizations can mitigate these issues, consolidated platforms are not foolproof yet.
6. Ever-Evolving: Some platforms are still evolving in terms of configurability, breadth of offerings, integration capabilities and more. Because consolidation is a newer concept, many vendors are still working out the kinks and are not infallible.
7. Narrow Client Base: Vendors often face difficulties in establishing trust as some platforms are yet to secure a robust healthcare client base. Consequently, their operational experience is limited to a narrow range of plan types and geographic areas.
8. Vendor Oversight: Some platforms prioritize strategic acquisitions over thorough integration and testing. This approach often results in solutions that perform poorly, with vendors opting to cover up these deficiencies by acquiring additional technologies and organizations rather than addressing underlying problems. To mitigate this, it is important to thoroughly research vendors when choosing to switch systems.
In Closing...
Healthcare organizations must harness the momentum of platforms, embracing unified solutions that may still be evolving. This proactive approach is critical, allowing both organizations and vendors to ‘learn by doing,’ facilitating mutual growth. Benefits extend beyond cost savings, paving the way for establishing long-term relationships with vendors. Simultaneously, it enables vendors to refine and bolster their offerings in collaboration with a variety of healthcare entities.
Given the substantial investment required for such transitions, selecting the right vendor is important. Organizations should assess their needs, timelines, budgets, and the broader market context. Additionally, in these large-scale, high-stakes implementations, it is essential to identify requirements and establish robust contractual agreements as it would ensure mitigating the risk of ‘laying all eggs in one basket’.
__________________________________________________________________________________________________________
- Software Analyst, 2023
- Workato
- Salesforce: Automation keeps Spotify’s Ad Business Growing Year over Year
- Kepler Cannon analysis
- Harvard Business Review: What’s Lost When Data Systems Don’t Communicate, 2023
- 20Becker’s Payer Issues: Top challenges, and opportunities facing the insurance industry in 2024
- LinkedIn: Impact of System Integration for your Business Operations, 2023
- O’Reilly, Data Quality Fundamentals, 2022
- Harvard Business Review
- Disjointed Software Dilemma, Medium, 2023
- Penalties for Violating HIPAA, ADA
- Kepler Cannon Analysis