The Future of Care
The healthcare industry is notorious for being resistant to change, perhaps because clinicians and patients prefer to stick to known courses of action. Lives are at stake after all, and there is not enough time to adjust to external changes. This explains why widespread digitization of patient records occurred only between 2010 and 2015, brought on by changes in regulation, decades after the introduction of computer technology.
The market landscape for core medical IT suggests that health tech is still at a nascent stage today. It is largely shaped by digitization and packaging of patient data for various hospital departments demonstrating an “institution-first” approach. However, this is set to change due to the growing rhetoric on value-based care that is patient centric and focused on quality rather than quantity. Innovations have started to mushroom to support this vision, including AI-enabled precision medicine, diagnostics and health monitoring wearable devices, giving the world a glimpse into the future of health.
An indication of the most promising innovation can be gauged by the investment activity in this space that is driven by three principles:
a. Continuous quality improvement
b. Cost optimization
c. Care everywhere
Companies that produce technology to meet these three principles are at the frontier of innovation.
Continuous Quality Improvement
Each patient visit generates a wealth of health data which is invaluable in provisioning evidence-based care. Intelligent data capture and storage coupled with the employment of advanced technologies is critical for improving systems and processes and delivering insights that can dramatically improve patient outcome and quality of care. To keep ahead of peers, providers need to establish a data management strategy and partner with producers of futuristic technology focused on improving quality of care.
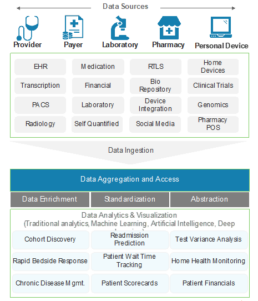
Data Management
The foundation of a sound data management architecture is an optimal data ingestion mechanism. Data production in healthcare occurs in different volumes, velocities, and formats by multiple sources – EHR, diagnostic, imaging, claims, billing, medical devices to name a few. It is essential to have an ingestion strategy that overcomes inherent silo-ization and harnesses all forms of data (structured, semi-structured and unstructured) into actionable assets.
One scenario is building a data pipeline for HL7 data format-framework for exchange, integration, retrieval of health information- by leveraging Big Data tech stack. This would provide health system 360° visibility into health records through integration and transformation of data into a single format with the added ability of querying it for deeper insights. Kafka and other distribution messaging technologies are examples of platforms that make high scale, flexible, real-time data integration possible.
In addition, a core platform that acts as a single source of truth for all stakeholders is essential for a complete data management strategy.
Pervasive AI
Progressive healthcare demands effective disease prevention, detection and treatment. This is achievable when data produces actionable next steps and predicts future outcomes. The impact of AI is expected to be revolutionary in three ways:
a. Proactive health management rather than disease treatment
b. Elevated clinical decision making through precision medicine
c. Supporting and meeting shortfall of medical practitioners
Exhibit 1. Key Principles Driving Healthcare Investments
In the near term, there will be increasing focus on optimizing results from continuously trained AI systems that identify and address anomalous cases differently from those that they are familiar with. This would achieve the next level of targeted and personalized care.
Some areas are witnessing deepening interest from the developer community of AI SaaS, as they demonstrate wider impact on population health. In precision medicine, AI is developing tailored therapies based on patient’s genome, historical health records and other data. For example, Viz.ai is using AI to detect and alert stroke teams of suspected large vessel occlusion strokes, enabling patients to get treatment faster. Their workflows improve access to life-saving care and deliver higher quality through early treatment and long-term disability prevention.
In population health management, AI is assisting infection control by tracking compliance with hygiene protocol, detecting infection outbreak, and predicting at-risk patients. Adoption of these AI-driven systems can help hospitals and health systems guide and control community-based health and disease metrics.
New-Age Medical Hardware
Early successes in AI integrated medical hardware have been demonstrated in diagnostics, surgery, and patient monitoring. These fields will pave the way in making medical devices more accurate, reliable, and intelligent.
AI is boosting precision in diagnostics through its application in imaging. Tencent AI Medical Imaging is a successful example. Currently, it is used for screening diseases including colorectal cancer and esophageal cancer. Advancing image recognition technologies have increased recognition accuracy to 90% for esophageal cancer and 97.2% for colorectal cancer1. These technologies will significantly reduce the 12 million diagnostic errors recorded annually in the US.2
Surgery in the future will be driven by robotics, be minimally invasive demonstrating high levels of precision. Monteris Medical has designed NeuroBlate which is a minimally invasive, MRI guided, robotic laser ablation system designed for use in the brain. Vicarious Surgical produced a VR-enhanced robotic surgical system that was awarded Breakthrough Designation by the FDA in 2019.
AI+IoT will drive patient monitoring and patient adherence to treatment protocols to improve clinical outcomes. Philips Healthcare’s Intellivue Gaurdian Solution uses cableless sensors on a patients’ wrist to track vital signs, the software then tracks and notes any deviation that indicates life-threatening crisis based on predictive modelling, alerting caregivers for early and effective intervention.
Cost Optimization
Healthcare costs are adding $155 billion to the cost of care annually3. A key driver of rising healthcare costs includes fee-for-service reimbursement that rewards volume of care rather than quality. Indirect cost reduction will be delivered through increasing precision in clinical intervention resulting in avoidance of unnecessary procedures and medication. Direct cost reduction initiatives involve a reimagining of the operating model for care provision and tech-based optimization of administrative workflow.
Operating Model Transformation
Some newer business models are adopting a team-based approach towards care. Strategic labor decisions that shift burden of care from physicians to cost-effective health workers – such as Behavior Health Specialists and Health Coaches- are driving down costs while maintaining high standards of care. Boston-based IORA health has designed a different kind of health system by building a primary-care provider network consisting of health coaches to handle patient observation and care. Care teams, comprising of a provider, Health Coach, Behavioral Health Specialist, Team Nurse, Clinical Team Manager and an Operations Assistant, work together to provide treatment.
Health coaches see patients more frequently than physicians and track patients’ progress on their behalf. The proven model reports a steep decrease of over 40% in hospitalization from better engagement and health management.
Administrative Workflow Optimization
High-volume, critical, “lights-on” administrative tasks across revenue cycle, supply chain, IT, HR, finance, accounting, and pharmacy operations are increasingly being run in the background through automated workflows.
In the case of payments administration which contributes to 14% of total healthcare expenditure, 5-10% of medical claims are fraudulent, resulting from over-billing or billing for a procedure that was not performed4. These inefficiencies are being eliminated through automation and transparency using blockchain, machine learning and RPA. For example, by automating the adjudication and payment process, blockchain stands to eliminate intermediaries and manual reconciliation processes.
Gem and Capital One partnered and developed a blockchain based solution to streamline payment administration, eliminating traditional claims clearing houses and reconciliation layers, lowering administrative costs, reducing revenue loss, and compressing cash flow cycles.
Olive combines RPA, computer vision, and machine learning to automate administrative workflows. Olive’s new Help technology is a desktop application that uses sensors to understand the context an employee’s work through the interaction they have with applications, webpages, and other virtual footprints. The solution then searches for relevant intelligence and delivers it to employees to support their jobs.
Care Everywhere: All Pervasive Patient Engagement
Patient engagement is moving beyond self-service kiosks and patient portals to omnipresent technology that monitors and guides patient health. Accelerated by the pandemic, the most significant change that the new decade welcomed is the widespread adoption of virtual care delivery. While certain aspects of virtual care have sprinted ahead –
Exhibit 2. Data Management Strategy
Telehealth- other supporting pillars such as remote patient monitoring and technologies “nudging” virtuous patient behavior are expected to quickly follow. This area is expected to record higher innovation quotient as physician and patients become more accustomed to giving and receiving virtual care.
Telehealth
Telehealth, the central pillar of ubiquitous care, goes beyond telemedicine. It includes other clinical services requiring connection between doctors, medical devices and patients and supporting non-clinical services such as provider training, administrative meetings, and medical education. As telehealth takes center stage, it is expected to become the first layer of the future care delivery ecosystem.
Examples of the reach and impact of innovators in this space include Teladoc, which completed more than 4.1 million telehealth visits in 2019 globally. It provides virtual health care services to employers, health plans, hospitals, health systems and insurance companies. RelayOne technology streamlines communications between surgical teams and third-party medical device vendors. Enduvo allows companies to create interactive and immersive AR and VR training for their business. Its no-code platform allows companies to easily create and distribute content to people on any device, including tablets, computers, and augmented and virtual reality devices.
Remote Patient Monitoring
Remote monitoring results in savings of $2,300 per patient per year, through the avoidance of complications and costly hospital admissions. If we multiply that by the 150 million Americans who have conditions best cared for through RPM (obesity, diabetes, COPD, behavioral health, etc.), it can deliver savings of $345 billion each year5. RPM is the embryo of the future healthcare ecosystem which would have a robust outpatient segment leveraging home-based care.
As an example, Optimize Health has developed end-to-end RPM service. When providers see that a patient at home needs support as indicated by a blood pressure cuff or a pulse oximeter, their software helps contact the patients through text messages and video calls. The company’s dashboard also provides a way to trigger a bill to the insurer. The system integrates with the underlying Electronic Health Record (EHR).
Other innovators such as Preventice Solutions and Biofourmis, have developed remote monitoring for chronic cardiac patients and a suite of wearables and software for remote monitoring, respectively. The latter raised $100 million this September which included funding by SoftBank Vision Fund 2.
Behavioral Change
The vision to convert healthcare to good health will largely be supported by virtuous changes in patient behavior towards self-managed care. Firms are now providing services that “nudge” them in the right direction. Amwell, a telemedicine provider, is interacting with patients through “nudges” and synchronous communication to promote compliance with healthy behaviors. Livongo, a digital tool provider for chronic condition management, has been trying to find the right balance and avoid “alert fatigue”. Based on consumer research, it has rolled out five-day health challenges, which is enough time to trigger behavioral changes. The intent of these products is to learn about their subscriber’s behavior to determine the kind of behavioral changes that might be most helpful for better population health outcomes.
Value A Giant's Vision for Healthcare
Apple, Google, Amazon—they all seem keen to play a much bigger role in healthcare. The scale of their businesses provides them resources much greater than traditional MedTech firms.
Their partnerships, investments and products will contribute significantly to the future of healthcare. At a high level, their collective vision is to initially support the traditional institution-first care, and eventually sidestep it with a human-first paradigm that promotes preventive self-managed care.
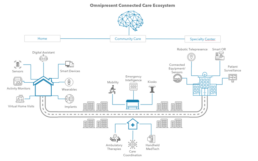
Exhibit 3. Omnipresent Self-Managed Healthcare
Steps to achieving this include combining traditional and new age sources of data for a complete picture of health, leveraging AI to augment personal and clinician decisions, creating a tightly integrated service value chain
Google has long had ambitions to expand into healthcare, however they have made a material impact only in the past few years.
It has sought to enter through cloud partnerships with health systems such as Ascension and Mayo clinic, provision of AI SaaS, and a robust partnership with DeepMind Health. In the absence of a formal Google vision for healthcare, its investments to date indicate the creation of a personal Google assistant for health. It is expected that it will combine EHR with data recorded from “non-invasive” devices and ambient sensors to create a patient-centered care cocoon. Before raising eyebrows around patient data security, Google was on the fast lane to produce EHR search engine and workflow simplification in partnership with Ascension Health. Essentially, their intent was to put a Google search bar at the top of every EHR that would allow users to search through records, including scanned documents and hand-written notes. Additionally, Google Health’s search bar would utilize existing Google technologies such as autocomplete and autocorrect to overcome human error such as misspelled words or non-identical matches.
In telehealth, Socratic, its education app, has included videos that couple with AR-glasses surgeons can use to train on medical devices. For developments in precision medicine, it has leveraged federated learning at Tensorflow, to overcome the requirement of a large health database by training algorithms on fragmented datasets- combining AI with HIPAA-mandated data privacy.
Additionally, Verily, Google’s health-centric sister company, in partnership with Swiss Re plans to provide stop-loss insurance.
The data-driven solution could disrupt the health insurance industry, by increasing patient engagement, speeding up intervention, and lowering costs of care
At a high level, Google is particularly well poised to stand out in healthcare by combining data sources and applying its AI capabilities, infiltrating healthcare through disease detection, data interoperability, and health insurance. It is the most active among big tech rivals in acquiring and investing in AI talent and applications. Since its first round of funding in 2009, Alphabet’s venture arm, Google Ventures (GV), has backed nearly 60 health-related enterprises ranging from genetics to telemedicine.
Apple
Apple’s vision for healthcare is personalized, proactive and preventive. It aims to build an integrated network of personal devices that collect, record, and analyze information continuously in the background, eliminating the need for hospital visits and reducing misdiagnosis. Its strategy is supported by three pillars hardware, i.e., the iPhone ecosystem, software, including ResearchKit and Carekit, and services like Fitness+.
The iPhone ecosystem (iPhone, Apple Watch, and AirPods) is being upgraded to include features for health monitoring. The iPhone has introduced the A-12 bionic chip which powers AI, dot projection for facial recognition, that would help in detecting conditions like autism. It is expected to use machine vision for additional health analysis. A new patent details how AirPods will be upgraded to capture biometric data (internal temperature, oxygen consumption levels, etc).
It is enabling health application development through FHIR and provisioning of health record API to third-party developers through its software development kit, HealthKit and CareKit. It allows patients to integrate health record data and provision data access to chosen applications. The kit provides ready templates that allow developers to quickly develop solutions.
There are indications of possible entry into primary care provision. In a research study, it introduced provider outreach via American Well, a telemedicine company. It may not be long before it combines health data with virtual communication for a complete care journey outside the traditional healthcare setup.
Amazon
Amazon has made selective and apparently disjointed and chequered forays into healthcare, indicating that it is still testing waters. Its initiatives include extension of its current business model and a few disruptive endeavors.
Its acquisition of PillPack, an online pharmacy, is an example of entry into healthcare via a known channel. Amazon has developed a sticky client base by revolutionizing customer experience, PillPack reflects similar strengths through its high NPS score.
In addition, Amazon has gained a built-out pharmacy supply chain and pharmacy licenses in all US states. Further, it can also leverage this business to expand to other disparate areas of healthcare through meaningful partnerships. For example, it can partner with telehealth service provider, create a single sign-on space in partnership with EHR system and partner with insurers to offer pharmacy services to its plan members.
Amazon Care is a disruptive initiative in primary care. Launched during the Covid-19 pandemic, it was conceptualized as a virtual health program for a selected base of employees with telehealth visits and in-person follow-up care.It became a successful in-house experiment with potential to be scaled out for the rest of its employees and employees of other firms through partnerships.
Amazon Comprehend Medical is an outgrowth of AWS, which provides NLP and AI services. It offers not only transcription services, and automated data population but also standardization of data for easier user access. Amazon HealthLake, its latest launch, is a data platform that stores, transforms, and analyses up to petabytes of life sciences data in AWS. It will apply intelligence across data silos, leveraging natural language processing and ontology mapping for supporting clinical decisions.
Meanwhile, Haven, the joint venture between Amazon, Berkshire Hathaway and JP Morgan Chase has wound up.
Exhibit 4. A Peak into the Giant’s Mind
Its mission statement envisioned the provision of affordable, high quality and transparent healthcare to their collective body of employees. While this initiative was in line with the principle of value-based care, its implementation lacked planning and strategy. The in-scope population of 1.2 million employees was spread across the geography, unable to accumulate market power to influence provider prices.
Additionally, the current incentive structure is heavily dependent on volume-based fee-for-service reimbursement rather than a capitation model that pays providers a fixed amount per member per month and is tied to health outcomes. This treats sickness rather than prevents it, rewarding increases in cost-of-care. Finally, individual forays including Amazon Care offering similar value may have accelerated its disbanding.
Exhibit 4. A Walk through the Future
In all, Amazon’s early vision for healthcare prioritizes transforming patient experience by seamlessly integrating synergistic services across the healthcare value chain with a focus on value-based care. It appears that it intends to achieve this by creating a virtual twin of its customer base through access to their health data.
Future Care Ecosystem
The Care ecosystem will soon become an integrated network of infrastructure exhibiting synchronized functioning for care delivery. In this network, home will become the key node for constant health monitoring and early care provision. The care infrastructure within homes will be enabled by a combination of IoT monitoring devices (smart toilets, smart mirrors, etc.), telehealth and AI driven clinical software analyzing health data and generating alerts.
Outside of homes, local hubs for retail care will develop which would include in-patient and out-patient facilities at a smaller scale.
Finally, there would be specialty centers catering to specific procedures which can only be performed and monitored within intensive care facilities. Additional elements, such as virtual communities defined by geography and health conditions will form, as a medium for population health management.
From an infrastructure standpoint, as the universe of acute inpatient services shrinks, and outpatient and home-based care provision increases, hospitals are likely to take less physical space. Hospital rooms will have body-worn and non-contact sensors enabling digitization of health information at source.
This would be connected to futuristic systems running advanced algorithm to glean and analyze health information. There will also be reduced administrative wait times due to the employment of robotic telepresence system- telehealth built specifically for administrative workflow management within hospitals. These are multi-functional, portable- audio visual enabled robotic systems connecting patients with physicians for periodic check-ups eliminating need for physical presence of physicians in the examination room. In most scenarios, it is expected that a large portion of care would be provided far away from hospitals.
Individual health will be tracked and monitored round the clock by AI. Robots and robotic systems will become ubiquitous from reception to detection and communication will be driven by virtual means providing wider care coverage for populations.
Preparing for the Future
A smooth transition to a future that sustains population wellness through AI-powered systems, remote health monitoring, and virtual care provision, requires providers to lay organization wide practices that support this change. There are four steps for implementing a successful transformation:
a. Defining your digital strategy
This involves addressing the changing landscape of people, process, and premise. The goal should be to upgrade clinical and non-clinical processes and care infrastructure with new technology. Further, it is essential for this program to be managed by the correct talent and external partners, requiring health systems to revisit their talent acquisition and partnership strategy.
b. Investing in data management
Bringing order to the chaos of information is an essential investment for modernizing the healthcare value chain. We recommend Providers invest in data integration platforms enabling capture, storage, security, and computing capability. Newer ways of Master Data Management will help overcome data fragmentation and duplication while establishing a single source of truth for information. A unified view of provider data across the enterprise will improve collaboration and quality of care and reduce costs.
c. Setting up enterprise middleware
Health systems should also set up a middleware that connects disparate applications into a single user interface enabling data interoperability. As consumers have experienced in retail and financial industries, middleware can problem solve by bringing about uses of data. It also ensures that new and legacy systems work together as organizations undergo digital transformation.
d. Partnering with innovators
Health systems should proactively partner with innovators to develop new solutions in line with their strategic priorities. This can take the shape of informed ideation of new products and services, early navigation of regulatory barriers, and planning for the integration of innovations with existing workflows.
In Closing...
It is essential for providers to build and pursue a vision that places patients and their service experience at the center of care provision. Building a foundation of sound data management, defining a digital strategy, architecting single user interface through interoperability, and partnering with others to build a modern MedTech stack are the surest ways to staying ahead of the curve.
1.Global Innovation Index, World Intellectual Property Organization
2.Singh H, Meyer AN, Thomas EJ. The frequency of diagnostic errors in outpatient care: Estimations from three large observational studies involving U.S. adult populations.
3.Department of labor Inflation report, 2019.
4. Herland M, Bauder R. Approaches for identifying U.S. Medicare fraud in provider claims data
5. Andelman J, “Why We Invested in Optimize Health”, Bonfire Ventures